Understanding ``Egg`` Lingo!
Undergoing fertility treatment is can be a challenging time. With so many procedures, treatments and technical terms to familiarize yourself with, you can end up feeling a little lost. Wilcox Fertility wants to help you and your partner feel secure and empowered, which is why we strive to educate you on all aspects of fertility treatment. This includes understanding the difference between “immature” and “mature” eggs.
If you’re undergoing fertility treatment such as in-vitro fertilization (IVF), you may have heard these terms. These expressions may sound as if the eggs were retrieved too early (or too late) during the ovarian stimulation process. However, this is not the case.
More often than not, if a woman’s eggs are considered “immature,” there is typically an underlying issue relating to fertility separate from the IVF process. Some reasons may be advanced maternal age, a diminished egg reserve, or polycystic ovarian syndrome (PCOS). These components can prevent an egg from reaching maturity and will most likely produce an embryo that is considered “aneuploid.” Aneuploid means the embryo carries an abnormal number of chromosomes.
Between the administration of your “trigger” shot, known as hCG (Human Chorionic Gonadotropan), and your egg retrieval, the total number of chromosomes in the nucleus of your egg decreases through “meiosis” or “maturational division.” This reduction means if you began with 46 chromosomes, it then reduces to 23 chromosomes. Fertility specialists can detect this change under a microscope, indicating the egg has reached maturity. However, if meiosis doesn’t take place, the egg is considered immature and incapable of developing into an embryo. That can have a tremendous impact on successful embryo implantation, and a live birth with chromosomal normality.
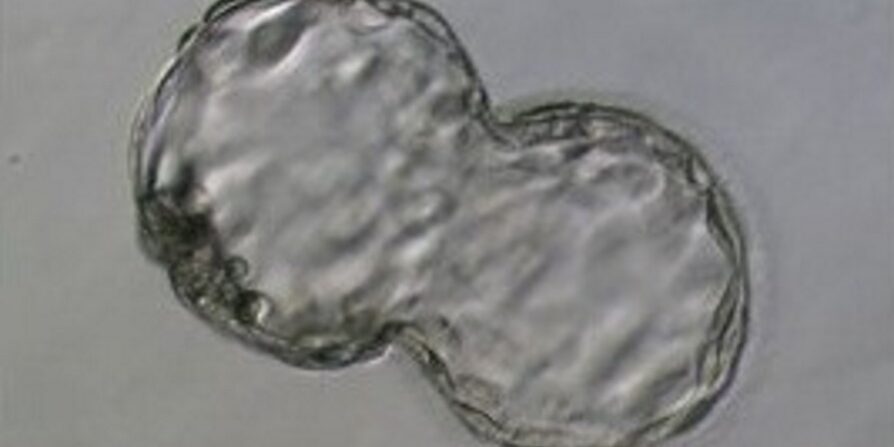
Similar to the above with eggs, sperm also need to undergo the same process of reducing their chromosomes from 46 to 23. Therefore, when the sperm is mixed with an egg as part of IVF, the resulting fertilized embryo will have 46 chromosomes needed to create a “euploid” embryo. A euploid embryo contains the correct number of chromosomes.
Embryos with less or more than 46 chromosomes (aneuploid) are at a lower risk of implantation in the uterine lining, and are at a higher risk for miscarriage or may result in a chromosomal developmental defect such as Down syndrome. It’s important to note, though, that even if a fertility specialist can identify a mature egg under a microscope, this is no indication that it has 23 chromosomes.
Euploid embryos, which contain the correct number of chromosomes, have a higher chance of implanting in the uterus and are most likely to lead to a live birth.
The best way to help determine if an embryo is aneuploid or euploid is through the help of genetic testing, such as Preimplantation Genetic Testing for Aneuploidy, previously known as PGS. This test can assist Dr. Wilcox in determining which embryos should be transferred providing you a greater chance of a healthy pregnancy and live birth.
Whether it’s understanding the medical terms of infertility or what tests you should consider, Dr. Wilcox and his team will be there to support you, and discuss each option. For more information on the numerous fertility treatments and family-building options offered at Wilcox Fertility, please continue to review other areas of our site or to inquire about financial details, don’t hesitate to contact us via our online form or call us at 626.657.9327.